Physician Credentialing stands as a critical foundation for a healthcare facility’s integrity and overall standing in the community. Despite its significance, the journey toward seamless and punctual credentialing is fraught with challenges. Here, we delve into four primary hurdles that complicate the credentialing process, often leaving hospital and practice management teams across the nation in a quandary.
Credentialing embodies one of the healthcare sector’s most detail-oriented administrative tasks. This rigorous process is pivotal for reimbursement procedures, yet it becomes a daunting challenge for facilities lacking seasoned administrative professionals capable of executing the necessary background checks with the required precision.
The duration of credential verification for a physician spans between 90 to 120 days, a period during which the physician remains unable to join any health plans. Consequently, any healthcare services offered by the physician within this timeframe go unreimbursed—either resulting in a financial write-off or pending claims. Such delays in credentialing can significantly impact a facility’s revenue flow, underscoring a misleading assumption that the credentialing process is flawlessly tight-knit. Yet, the reality unveils a spectrum of obstacles shadowing credentialing, leaving many healthcare organizations striving to achieve timely and hassle-free physician credentialing.
Here are the top 4 challenges that make the credentialing process so arduous:
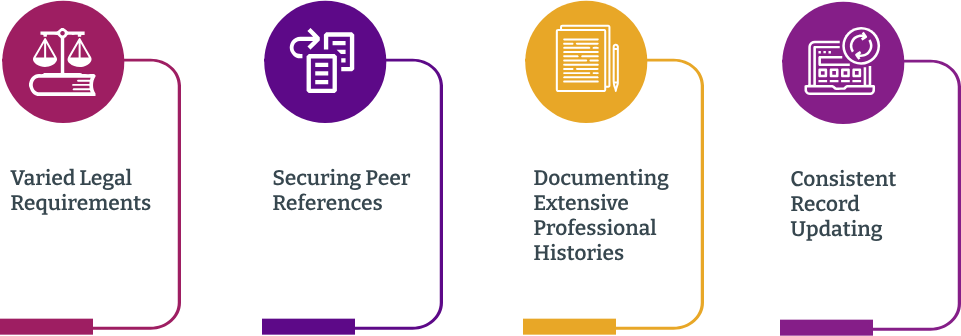
Varied Legal Requirements – The credentialing criteria fluctuate across different accrediting bodies and states, making it a complex task to pinpoint and aggregate the precise documents required for submission. Adopting a credentialing-specific Saas platform to oversee your credentialing efforts can be an effective strategy to navigate through this maze.
Securing Peer References – An essential component of the credentialing dossier, peer references can be particularly challenging to obtain due to the heavy workloads of referencing physicians. A proactive measure is to ensure all other prerequisites are complete before reaching out to peers, fostering a smoother process and minimizing additional burdens on them.
Documenting Extensive Professional Histories – Assembling the career timeline of a seasoned physician is not without its trials. Facilities previously associated with these professionals may no longer be operational, adding layers of difficulty to the verification process.
Consistent Record Updating – Given the statutory mandate for periodic re-evaluation, credentialing becomes a recurring task. Keeping systematic records of past verifications is vital to ensure a streamlined process for future credentialing efforts.

Madaket Health’s Provider Data Management (PDM) platform offers a comprehensive solution to the complexities surrounding credentialing due to fluctuating criteria across various accrediting bodies and states. By automating manual and error-prone processes, Madaket Health streamlines the aggregation and submission of the necessary documents for credentialing. This platform is designed to simplify the often cumbersome task of ensuring that healthcare providers meet the diverse credentialing requirements mandated by different accrediting organizations and jurisdictions.
One of the significant benefits of using Madaket’s PDM platform is its ability to manage and exchange data for key healthcare administrative functions, including payer enrollment, credentialing, and licensing. This system reduces the burden on health systems by providing a unified platform that supports the precise identification and aggregation of required documentation, making the credentialing process more efficient and less prone to error.
Through partnerships and integrations, such as with Licentiam and Mocingbird, Madaket expands its credentialing and continuous medical education (CME) management capabilities within its cloud-based platform. This ensures that health systems can navigate the credentialing process more smoothly, regardless of the varying and evolving criteria across states and accrediting bodies. By leveraging Madaket’s PDM platform, healthcare systems gain a strategic advantage in managing the complexities of provider credentialing, leading to improved compliance, faster provider onboarding, and ultimately enhancing the quality of patient care.
Schedule a demo to see how Madaket Health’s PDM platform can simplify and streamline your credentialing process, ensuring compliance and efficiency.
© 2024 Madaket Health | Privacy Policy | Terms & Conditions